Dental hygiene is a specialized field focused on maintaining oral health through preventive care and educational practices. It plays a crucial role in promoting overall well-being by addressing gum diseases, tooth decay, and other oral conditions. The foundation of dental hygiene lies in understanding the connection between oral health and systemic diseases, emphasizing the importance of regular dental check-ups and proper hygiene routines. Historically, dental hygiene practices have evolved significantly, transitioning from basic cleaning methods to evidence-based treatments, highlighting its growing relevance in modern healthcare.
1.1 Definition and Scope of Dental Hygiene
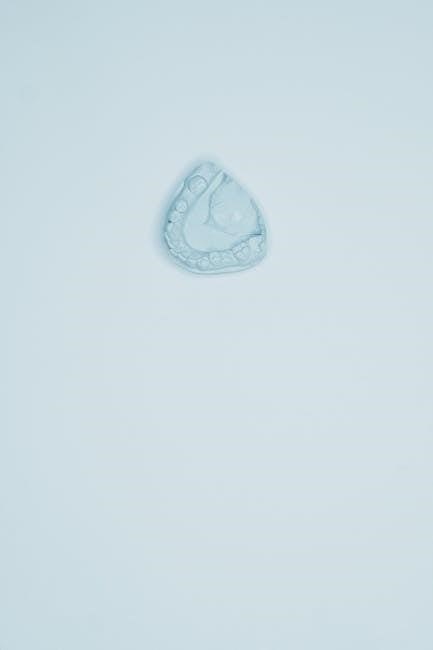
Dental hygiene refers to the practice of maintaining oral health through preventive measures and therapeutic interventions. It is a specialized field within dentistry focused on preventing and treating conditions affecting the teeth, gums, and surrounding tissues. The scope of dental hygiene includes clinical procedures such as scaling, polishing, and fluoride application, as well as patient education on proper oral care. Dental hygienists play a critical role in early detection of oral diseases, enabling timely interventions. The field also encompasses assessing patient needs, developing personalized treatment plans, and promoting public health initiatives. By addressing oral health, dental hygiene contributes to overall well-being, linking it to systemic health conditions like heart disease and diabetes. Advances in research and technology continue to expand the scope of dental hygiene, making it a dynamic and essential component of modern healthcare.
1.2 Importance of Dental Hygiene in Overall Health
Dental hygiene is essential for maintaining overall health, as poor oral health can lead to systemic diseases. Research shows links between gum disease and conditions like heart disease, diabetes, and respiratory infections. Neglecting oral care can result in chronic inflammation, which may worsen these health issues. Additionally, dental hygiene plays a role in mental well-being, with a healthy smile enhancing self-esteem and quality of life. Regular dental hygiene practices prevent bad breath, tooth loss, and pain, ensuring proper nutrition and social confidence. By addressing oral health, individuals can reduce the risk of broader health complications, emphasizing the importance of dental hygiene in holistic well-being.
1.3 Brief History of Dental Hygiene Practices
The history of dental hygiene practices dates back thousands of years, with early civilizations employing various methods to maintain oral health. Ancient Egyptians and Chinese used chewing sticks with frayed ends to clean teeth, while Greeks and Romans utilized cloths and ground bones. The first toothbrush, made from boar hair, emerged in China during the 1200s. Modern dental hygiene began to take shape in the late 19th century with the establishment of the first dental hygiene school in 1913 by Alfred Fones. Early practices focused on scaling and polishing teeth, with fluoride treatments and preventive care gaining prominence in the 20th century. These advancements have evolved into the evidence-based practices seen today, emphasizing prevention and patient education to promote lifelong oral health.

Key Components of Dental Hygiene
Daily oral care routines, including brushing and flossing, are essential for maintaining oral health. Regular dental visits and proper nutrition also play a vital role in preventing diseases.
2.1 Daily Oral Care Routine
A daily oral care routine is essential for maintaining good oral health. It typically includes brushing teeth twice a day with fluoride toothpaste, using gentle circular motions to remove plaque and bacteria. Flossing once daily helps remove food particles and plaque between teeth and under the gumline, areas a toothbrush cannot reach. Rinsing with water or mouthwash can further cleanse the mouth and freshen breath. Additionally, replacing toothbrushes every three to four months ensures effectiveness. Consistency in this routine prevents plaque buildup, reduces the risk of gingivitis, and promotes overall dental well-being. Regular fluoride exposure strengthens tooth enamel and prevents decay, making daily oral care a cornerstone of dental hygiene practices.
2.2 Role of Brushing and Flossing
Brushing and flossing are fundamental components of oral hygiene, playing a critical role in removing plaque and food particles. Brushing teeth twice daily with a fluoride toothpaste helps eliminate surface bacteria and food residue, while flossing once a day targets interdental spaces and subgingival areas inaccessible to a toothbrush. These practices prevent plaque accumulation, which can lead to tooth decay and gum inflammation. Regular brushing also polishes tooth surfaces, reducing stains and enhancing aesthetic appeal. Flossing complements brushing by addressing areas prone to plaque buildup, thereby safeguarding against periodontal diseases. Together, these habits form the backbone of a preventive oral care regimen, significantly reducing the risk of dental problems and promoting long-term oral health. Consistent adherence to these practices is vital for maintaining a healthy, functional smile and preventing costly dental interventions. Regular dental check-ups further enhance their effectiveness, ensuring comprehensive oral care.
2.3 Importance of Dental Visits and Check-ups
Regular dental visits and check-ups are essential for maintaining optimal oral health and preventing potential issues. They allow dental professionals to identify and address problems early, such as cavities, gum disease, or other abnormalities, before they escalate into more severe conditions. Professional cleanings remove plaque and tartar that brushing and flossing alone cannot eliminate, reducing the risk of periodontal disease. Additionally, dental check-ups provide an opportunity for personalized advice on improving oral hygiene practices. Early detection of issues like oral cancer or misaligned teeth can lead to timely interventions, improving treatment outcomes. Regular visits also promote better overall health, as research links gum disease to systemic conditions such as diabetes and heart disease. Consistent dental care helps prevent costly and invasive procedures, ensuring a healthy, functional smile for years to come.
2.4 Nutritional Impact on Oral Health
Nutrition plays a significant role in oral health, as the foods and beverages we consume directly impact our teeth and gums. Sugary and acidic foods contribute to tooth decay and enamel erosion, while a balanced diet rich in essential nutrients supports healthy oral tissues. Calcium, vitamin D, and fluoride are particularly important for strengthening tooth enamel and preventing decay. Additionally, vitamin C helps maintain healthy gums, reducing the risk of periodontal disease. A diet high in fiber can stimulate saliva production, which naturally cleanses the mouth. Conversely, poor dietary habits can lead to nutritional deficiencies, increasing susceptibility to oral infections and gum disease. Understanding the nutritional impact on oral health emphasizes the importance of making informed food choices to promote a healthy smile and overall well-being.

Dental Hygiene Tools and Instruments
Dental hygiene tools include manual and electric toothbrushes, dental floss, interdental brushes, mouthwashes, and fluoride products. Professional instruments like ultrasonic scalers and drills aid in thorough cleaning and maintenance, ensuring optimal oral hygiene and preventing dental issues.
3.1 Manual and Electric Toothbrushes
Manual toothbrushes are widely used for their simplicity and affordability, requiring manual dexterity to clean teeth effectively. Electric toothbrushes, with rotating or oscillating heads, often have pressure sensors and timers, enhancing cleaning efficiency. Both types are effective, but electric brushes may offer better plaque removal in challenging areas. The choice depends on personal preference and dental needs. Proper brushing technique is essential for both, ensuring all surfaces are cleaned without causing gum damage. Regular replacement of worn bristles is crucial for maintaining hygiene. Electric toothbrushes may be more suitable for individuals with limited dexterity, while manual brushes provide portability and ease of use. Each has its advantages, contributing to comprehensive oral care routines.
3.2 Dental Floss and Interdental Brushes
Dental floss and interdental brushes are essential tools for removing plaque and food particles from between teeth and below the gumline, areas a toothbrush cannot reach. Flossing daily helps prevent gingivitis and interproximal cavities by cleaning tight spaces. Interdental brushes are small, cone-shaped brushes designed for larger gaps or irregular spaces, making them ideal for orthodontic patients or those with periodontal pockets. Both tools are crucial for maintaining periodontal health and preventing bad breath. Proper technique is vital to avoid gum damage. Regular use of floss and interdental brushes complements brushing, ensuring a thorough cleaning routine. They are indispensable for achieving optimal oral hygiene and preventing dental issues before they escalate.
3.3 Mouthwashes and Fluoride Products
Mouthwashes and fluoride products are integral to oral hygiene, offering additional protection against tooth decay and gum disease. Fluoride toothpaste and mouthwashes strengthen enamel, making teeth more resistant to acid attacks from plaque and sugars. Antiseptic mouthwashes reduce bacteria, freshen breath, and combat gingivitis. Fluoride varnishes and gels are professionally applied for high-risk patients, providing long-lasting protection. Desensitizing mouthwashes alleviate sensitivity, while whitening products remove surface stains. Proper use of these products complements brushing and flossing, enhancing overall oral health. However, overuse or improper application can lead to issues like tooth discoloration or fluoride overload. Always follow dental recommendations for optimal benefits and safety.
3.4 Professional Cleaning Instruments
Professional cleaning instruments are essential tools used by dental hygienists to remove plaque, tartar, and stains, ensuring thorough oral cleaning. Ultrasonic scalers, which use high-frequency vibrations and water, are commonly employed for efficient plaque and tartar removal above and below the gum line. Hand scalers, with their curved blades, are used for precise cleaning in specific areas. Polishing tools, such as prophylaxis cups, smooth tooth surfaces and remove surface stains, enhancing the effectiveness of cleaning. Additionally, suction devices are used to remove debris and saliva, maintaining a clear field during procedures. These instruments play a critical role in preventing oral diseases and maintaining optimal oral hygiene, ensuring that dental cleanings are both effective and safe for patients.

Common Dental Hygiene Techniques
Common dental hygiene techniques include scaling, polishing, and fluoride application to prevent and treat oral conditions. These methods ensure effective plaque removal and cavity prevention, promoting oral health.
4.1 Proper Brushing Techniques
Proper brushing techniques are essential for maintaining good oral hygiene. Brushing should be done twice a day for two minutes each session, using gentle circular motions with a soft-bristled toothbrush. The brush should be held at a 45-degree angle to the gums, ensuring the bristles reach the gum line without causing irritation. Special attention should be paid to the front, top, and back surfaces of all teeth, as well as the chewing surfaces. Avoid using excessive force, which can damage gums and tooth enamel. Replace the toothbrush every three months or when the bristles become frayed. Using fluoride toothpaste and focusing on areas where teeth and gums meet are key to effective plaque removal and cavity prevention. Regular brushing helps maintain healthy gums and prevents common oral health issues.
4.2 Effective Flossing Methods
Effective flossing is a critical component of oral hygiene, removing plaque and food particles between teeth where a toothbrush cannot reach. To floss properly, wrap the floss around your middle fingers, leaving about 1-2 inches of floss between them. Gently guide the floss between teeth using a zigzag motion, curving it around the base of each tooth in a “C” shape. Avoid snapping the floss, as this can irritate the gums. Move to a new section of floss for each tooth to prevent transferring bacteria. Flossing should be done once daily, preferably before brushing, to ensure thorough removal of plaque. Regular flossing helps prevent gingivitis, bad breath, and interdental cavities, promoting a healthier smile and overall oral well-being.
4.3 Scaling and Polishing Procedures
Scaling and polishing are essential dental hygiene procedures aimed at removing plaque, tartar, and stains from teeth, both above and below the gum line. Scaling involves using specialized tools, such as ultrasonic scalers, to break down and remove hardened plaque (tartar) that can lead to gum inflammation and infection. Polishing follows scaling, using abrasive pastes to smooth tooth surfaces, reducing areas where bacteria can adhere. These procedures are crucial for preventing gingivitis and periodontal diseases, ensuring a clean and healthy smile. Regular scaling and polishing also help eliminate bad breath and improve the effectiveness of daily oral care routines. They are typically performed during professional dental cleanings, tailored to individual patient needs for optimal oral health outcomes.

4.4 Fluoride Application Methods
Fluoride application is a key dental hygiene procedure aimed at strengthening tooth enamel and preventing decay. Common methods include fluoride varnishes, gels, foams, and mouthwashes. Varnishes are painted directly onto teeth for prolonged contact, while gels and foams are applied using trays. Mouthwashes are used for at-home application. These methods enhance enamel resistance to acid attacks from plaque and sugars, reducing cavity risk. Professional applications are typically recommended for high-risk patients, such as children or those with a history of decay. Proper technique ensures maximum effectiveness and safety, making fluoride treatments a cornerstone in preventive dental care for maintaining healthy, resilient teeth and promoting overall oral health.

Infection Control in Dental Settings

Infection control in dental settings is crucial for preventing disease transmission between patients and staff. It involves sterilization, proper hygiene, and adherence to safety guidelines to ensure a safe environment.
5.1 Types of Infections in Dental Practices
Dental practices are susceptible to various infections, including bacterial, viral, and fungal. Bloodborne pathogens like HIV and hepatitis are significant risks due to exposure to bodily fluids. Airborne pathogens, such as tuberculosis, pose threats through inhalation. Contact infections occur via contaminated instruments or surfaces. Additionally, oral infections like caries and periodontal diseases can spread if not properly managed. Proper sterilization and hygiene practices are essential to mitigate these risks and protect both patients and staff. Understanding the types of infections helps in implementing targeted prevention strategies, ensuring a safer environment for dental care. Regular training and adherence to infection control protocols are vital in minimizing these risks effectively.
5.2 Best Practices for Infection Prevention
Effective infection prevention in dental practices relies on consistent adherence to evidence-based protocols. Hand hygiene is paramount, requiring the use of alcohol-based hand rubs or soap and water before donning gloves. Personal protective equipment (PPE), such as gloves, masks, and eye protection, must be worn during procedures to minimize exposure to bodily fluids. Instruments should be sterilized using autoclaves or chemical disinfectants, while surfaces should be disinfected regularly with EPA-approved products. Proper sharps handling and safe waste disposal are critical to prevent needlestick injuries and contamination. Patient assessment and medical history review help identify high-risk individuals, enabling tailored precautions. Regular training and compliance with IPAC principles ensure a safe environment for both patients and dental staff, reducing the risk of infection transmission.
5.3 IPAC Principles in Dentistry
Infection Prevention and Control (IPAC) principles are fundamental to maintaining a safe dental environment. These principles emphasize patient assessment to identify infection risks and implement tailored precautions. Routine practices, such as hand hygiene and use of personal protective equipment (PPE), are applied consistently to all patients. Sterilization and disinfection of instruments and surfaces are critical to prevent pathogen transmission. Dental teams must follow guidelines for sharps safety and proper waste management. IPAC also includes the use of barriers and PPE during procedures involving blood or bodily fluids. Regular training and adherence to these principles ensure compliance with public health standards, protecting both patients and dental healthcare providers from infectious diseases.
5.4 Antibiotic Prophylaxis Guidelines
Antibiotic prophylaxis in dentistry is reserved for specific high-risk patients to prevent infection during certain procedures. Recent guidelines, such as those from the ADA and AAOS, recommend prophylaxis primarily for patients with prosthetic joints, certain heart conditions, or immunocompromised states. The aim is to reduce the risk of implant infections or systemic complications. Over 80% of antibiotics prescribed for dental procedures are unnecessary, highlighting the need for stricter adherence to guidelines. This approach minimizes antibiotic resistance and ensures appropriate use. Dental professionals must assess each patient’s medical history and risk factors to determine if prophylaxis is indicated. Collaboration between dentists and physicians is essential for high-risk cases. These guidelines emphasize evidence-based practices to balance infection prevention with responsible antibiotic use.
5.5 Sterilization and Disinfection Methods
Sterilization and disinfection are critical in dental settings to prevent the spread of infections. Autoclaving is the most reliable method for sterilizing dental instruments, using high-pressure steam to kill pathogens. Chemical disinfectants, such as glutaraldehyde or hydrogen peroxide, are used for surfaces and equipment that cannot be autoclaved. Proper hand hygiene, including glove use, is essential for patient and provider safety. Dental units and water systems must be regularly cleaned and disinfected to prevent contamination. Sterilization protocols should follow CDC and ADA guidelines to ensure effectiveness. Regular monitoring and maintenance of sterilization equipment are necessary to uphold infection control standards. These methods collectively create a safe environment for both patients and dental healthcare providers.

Patient Assessment and Diagnosis
Patient assessment involves evaluating medical history, clinical examination, and radiographic evaluation to diagnose oral health issues. Accurate diagnosis guides personalized treatment planning, ensuring effective care.
6.1 Initial Patient Evaluation
The initial patient evaluation is a critical step in dental hygiene care, ensuring comprehensive assessment of oral health. It involves reviewing medical history, assessing chief complaints, and conducting visual examinations. Updating medical histories helps identify systemic conditions impacting oral health. Vital signs, such as blood pressure, are often recorded to ensure patient safety. This evaluation also includes discussing patient concerns and expectations. Effective communication builds trust and ensures personalized care. Accurate documentation of findings is essential for developing targeted treatment plans. The initial evaluation sets the foundation for subsequent diagnostic procedures, ensuring all aspects of patient health are considered. It is a dynamic process that adapts to individual needs, promoting optimal outcomes.
6.2 Medical History and Risk Assessment
Assessing a patient’s medical history is crucial for identifying potential risks and tailoring dental care. This step involves reviewing systemic conditions, allergies, and medications that may impact treatment. Conditions like diabetes or heart disease require special considerations, such as antibiotic prophylaxis. A thorough review helps prevent complications during procedures. Updating medical histories ensures accuracy and safety. Effective communication with patients is key to uncovering relevant information. Risk assessment also involves evaluating lifestyle factors, such as smoking or alcohol use, which can affect oral health. This process ensures personalized care and minimizes risks. By understanding the patient’s overall health, dental hygienists can provide safe and effective treatment. Regular updates to medical histories are essential for ongoing care. This step is vital for preventing adverse outcomes and ensuring patient safety.
6.3 Clinical Examination Techniques
Clinical examination techniques are essential for assessing oral health and detecting potential issues. Visual inspection is the first step, allowing hygienists to identify signs of decay, gingivitis, or other abnormalities. Periodontal assessment involves probing pocket depths to evaluate gum health and detect periodontal disease. Plaque and tartar are assessed to determine the need for cleaning. Dental charting records the condition of each tooth, noting restorations, missing teeth, or areas of concern. Radiographic images, such as X-rays, provide insights into underlying structures. These techniques help identify risks and guide treatment planning. Proper documentation ensures accurate records for future reference and legal purposes. Regular clinical exams are vital for early detection and prevention of oral health issues, promoting long-term patient well-being.
6.4 Radiographic Evaluation
Radiographic evaluation is a critical diagnostic tool in dental hygiene, providing detailed images of oral structures. It helps identify hidden conditions such as decay, abscesses, or bone loss. Common types include intraoral X-rays (e.g., bitewing, periapical) and extraoral X-rays (e.g., panoramic). These images aid in assessing periodontal health, detecting fractures, and evaluating the success of previous treatments. Radiographs are essential for comprehensive patient assessment and treatment planning. They complement clinical exams by revealing issues not visible during visual inspections. Regular updates ensure accurate monitoring of changes over time. Dental hygienists play a key role in interpreting these images to guide interventions, ensuring timely and effective care. Proper use of radiography adheres to the ALARA principle, minimizing radiation exposure while maximizing diagnostic benefits.
6.5 Diagnosis and Treatment Planning
Diagnosis and treatment planning are pivotal steps in dental hygiene care, involving the assessment of clinical findings, medical history, and radiographic results. This process identifies oral health issues, such as periodontal disease or caries, and determines the appropriate interventions. Personalized treatment plans are developed to address specific patient needs, ensuring effective and targeted care. Collaboration between dental hygienists and dentists is essential to create comprehensive strategies. The plan may include scaling, polishing, fluoride treatments, or referrals for specialized care. Regular monitoring and adjustments ensure the efficacy of the treatment. Accurate documentation of the diagnosis and plan is crucial for continuity of care and legal purposes. This step ensures that patients receive evidence-based, individualized care tailored to their unique oral health requirements.

Special Populations in Dental Hygiene
Dental hygiene care for special populations, such as children, geriatric patients, and medically compromised individuals, requires tailored approaches to address unique oral health needs and challenges effectively.
7.1 Dental Care for Children
Dental care for children focuses on promoting healthy oral development and preventing early childhood caries. Regular dental visits and fluoride treatments are essential. Parents should be educated on proper brushing techniques and dietary habits to minimize sugar intake. Age-specific preventive measures, such as sealants and fluoride varnishes, are recommended. Early detection of orthodontic issues and habits like thumb-sucking should be addressed; Creating a positive dental experience helps reduce anxiety and fosters lifelong oral health habits. Tailored approaches ensure individual needs are met, from infancy through adolescence.
7.2 Geriatric Dental Hygiene Practices
Geriatric dental hygiene focuses on addressing the unique oral health needs of elderly patients. Common issues include gum recession, dry mouth, and tooth wear. Regular dental check-ups are crucial for early detection of conditions like periodontal disease and oral cancer. Dentures and implants require proper maintenance to ensure comfort and function. Hygiene practices may need to be adapted for patients with limited dexterity or cognitive decline. Tailored care plans, including soft-bristle toothbrushes and gentle mouthwashes, can help maintain oral health. Additionally, addressing systemic health conditions, such as diabetes or arthritis, is vital for overall well-being. Educating caregivers on proper oral hygiene techniques can significantly improve outcomes for geriatric patients.
7.3 Dental Hygiene for Medically Compromised Patients
Dental hygiene for medically compromised patients requires tailored approaches to address their unique health conditions. A thorough medical history review is essential to identify risks and ensure safe care. Patients with conditions like diabetes, cardiovascular diseases, or immunodeficiencies may need specialized oral hygiene strategies. bleeding disorders or anticoagulant use necessitate cautious procedures to prevent complications. Infection control is critical, especially for immunocompromised individuals. Collaboration with healthcare providers ensures comprehensive care. Personalized hygiene plans, including gentle cleaning techniques and antimicrobial therapies, are often recommended. Regular monitoring and adjustments to treatment plans help manage oral health effectively in this vulnerable population.
7.4 Dental Care for Immunocompromised Patients
Dental care for immunocompromised patients requires heightened vigilance to prevent infections and manage oral health effectively. These patients, including those with HIV/AIDS, cancer, or organ transplants, are more susceptible to infections due to their weakened immune systems. Dental professionals must conduct thorough risk assessments and implement strict infection control measures, such as sterilization and barrier techniques, to minimize exposure to pathogens. Antibiotic prophylaxis may be recommended in high-risk cases to prevent complications. Personalized oral hygiene plans, including gentle cleaning and antimicrobial therapies, are essential. Regular monitoring and collaboration with the patient’s healthcare team ensure tailored care. Early detection and treatment of oral issues are critical to avoid severe complications in this vulnerable population.



